To My Daughters,
I remember a car ride years ago when one of your brothers was upset that he got a bad grade and was worried that he wasn’t ‘smart’. I told all of you that the most important qualities in a person (to me) are being kind and brave. You all got the gist of being kind but had some trouble envisioning what being brave looked like at your age. Your then-5 y/o-brother asked if it meant that he should act like a superhero and save the world from villains, but we discussed that it’s actually simpler than that. You can be brave on a regular basis in small (but impactful) ways like standing up for a kid who is being made fun of, or staying firm in establishing boundaries, even when others don’t like them. Bravery is having integrity (often quietly but sometimes fiercely) in situations, even when it feels hard or when others don’t.
As you know, I am both heartbroken and infuriated by the decision of the Alabama Supreme Court in mid-February where it ruled that three couples who had frozen embryos destroyed in an accident at a storage facility could pursue wrongful death lawsuits for their “extrauterine children.” Although once Roe V Wade was overturned, we (in the infertility field) knew that this decision might negatively affect us and our patients, I naively believed that they would leave IVF alone for now, since (last I checked) trying to build your family is pro-life. To me, being ‘pro-life’ implies that you care about the life of the child at all stages, not just before he/she is born. Apparently, ‘extrauterine’ in Alabama extends to protecting embryos in an IVF lab but not the babies born from these embryos once they live in the real world. Alabama (along with many of the other restrictive states) has one of the highest rates of infant mortality and ranks as one of the lowest states in terms of the health of the children who live there. Making laws that only protect fertilized eggs (but not the babies generated from them) is not ‘pro-life’, it is pro-birth. What is even more alarming is that this decision is just the beginning of a dangerous trend nationally, as there are over a dozen states that consider ‘life’ starting at the time of fertilization.
The Supreme Court of Alabama consists of a chief justice and eight associate justices who, at the time of this writing, are all Republican. Their political affiliation shouldn’t matter as long as they remain unbiased and don’t use their positions to further their political agenda and/or personal philosophy. The issue with this decision is that it reads as theocratical. Consider the following language in the ruling: “The People of Alabama took what was spoken of the prophet Jeremiah and applied it to every unborn person in this state” and “[Alabamians] have required us to treat every human being in accordance with the fear of a holy God who made them in His image”. In fact, the lead justice not only often invokes scripture in making legal decisions, but he criticizes those who don’t and supports an organization of conservative Christians who believe that we should use fundamentalist beliefs to influence and run government.
The Bible is not (nor was it meant to be) a legal textbook, and it’s a judge’s job to be objective and rely on case law and legal precedent even if they are philosophically uncomfortable or opposed to it.
As you know, I grew up Catholic. I believe in God and I feel strongly about respecting other people’s religious and spiritual beliefs. As a Nurse Practitioner, I’ve seen many examples of patients or couples who chose to alter their suggested treatment course based on their religious beliefs. In the case of one couple who needed IVF, they asked that only a few eggs (out of the many that were produced) be fertilized as they were uncomfortable with freezing extra embryos. We counseled them that reducing the number of embryos created may reduce the odds of achieving a pregnancy that cycle (necessitating subsequent cycles at their financial and emotional expense) but then happily complied after we were confident that they understood. In one of my other jobs, we allowed rabbis to be present during IVF procedures whenever patients requested this.
In medicine, decisions and strategies are based on current, peer-reviewed, published scientific data that is analyzed and replicated so that it’s appropriate and applicable to most. We should not be basing medical care on the Old Testament.
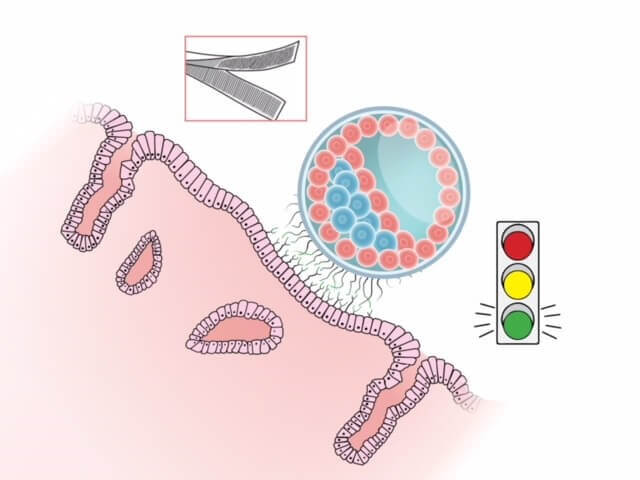
The stimulation of multiple eggs during an IVF cycle is necessary to counter the natural attrition rate from mature egg to fertilized egg to blastocyst (the term for an embryo at implantation). Only approximately 30-50% of fertilized eggs progress to the blastocyst stage and 30-90% of blastocysts are aneuploid (an embryo that has an abnormal number of chromosomes, which is usually not consistent with life). This translates to the need to create many eggs just to be able to have 1-2 chromosomally normal blastocysts available to transfer back in the hope that one of them will implant and become a healthy pregnancy. Restricting the number of eggs that we can fertilize (and/or the ability to freeze extra embryos) based on theology forces medical professionals to abandon common sense and years of scientific data.
Ok, let’s circle back to you (and your brothers). Even though I am deeply concerned about the effects of this court decision (and others like it), there are still ways to be a superhero.
Maybe your sword is your voice or your pen which you can use to advocate for those who are disempowered to advocate for themselves.
Maybe your superpower is being respectful and considerate to all people, regardless of their appearance, politics, religion, circumstances, or how much money they make.
Maybe your cape is your suit or robe should you decide to pursue a role as a lawmaker or politician where you advocate for others and make fair and reasonable decisions based on common sense, defensible facts, case law, and empathy, not your personal religious beliefs or political views.
I know I sometimes embarrass you by being a firm (and sometimes loud) advocate for reproductive health but being kind and brave means doing the right thing. Even when it’s the hard thing.
But, to channel Glennon Doyle, “We can do hard things”.
Love,
Mom